We Answer Common Questions About The D614G Mutation

Nope, D614G is not the latest breed of durians in town.
We hate to burst your bubble, but it is a mutation on the original COVID-19 virus. Simply put, SARS-CoV-2 got an upgrade, for better or for worse.

The recent announcement on 16th August by DG Datuk Dr Noor Hisham that the D614G-type mutation is detected in Malaysia has contributed to a wave of panic amidst the birth of new clusters nationwide.
The strain was detected from the Sivagangga patient-under-investigation (PUI) Cluster and a case from the Ulu Tiram Cluster.
Without further ado, let’s get to know D614G a little better.
Why do viruses mutate?
Viruses tend to upgrade (read: mutate) to become better versions of themselves as per natural selection. Viruses may also mutate due to random genetic drift.
In this situation, it is helpful to remember that viruses also mutate as part of their life cycle, and not all mutations are harmful. In fact, some mutations can also make viruses weaker.
The World Health Organisation (WHO) has published a bulletin on their findings of variant SARS-CoV-2 genomes, and as of May 2020, there were an astounding 5775 distinct genome variants, with 6 major clades and 14 subclades.
What is D614G?
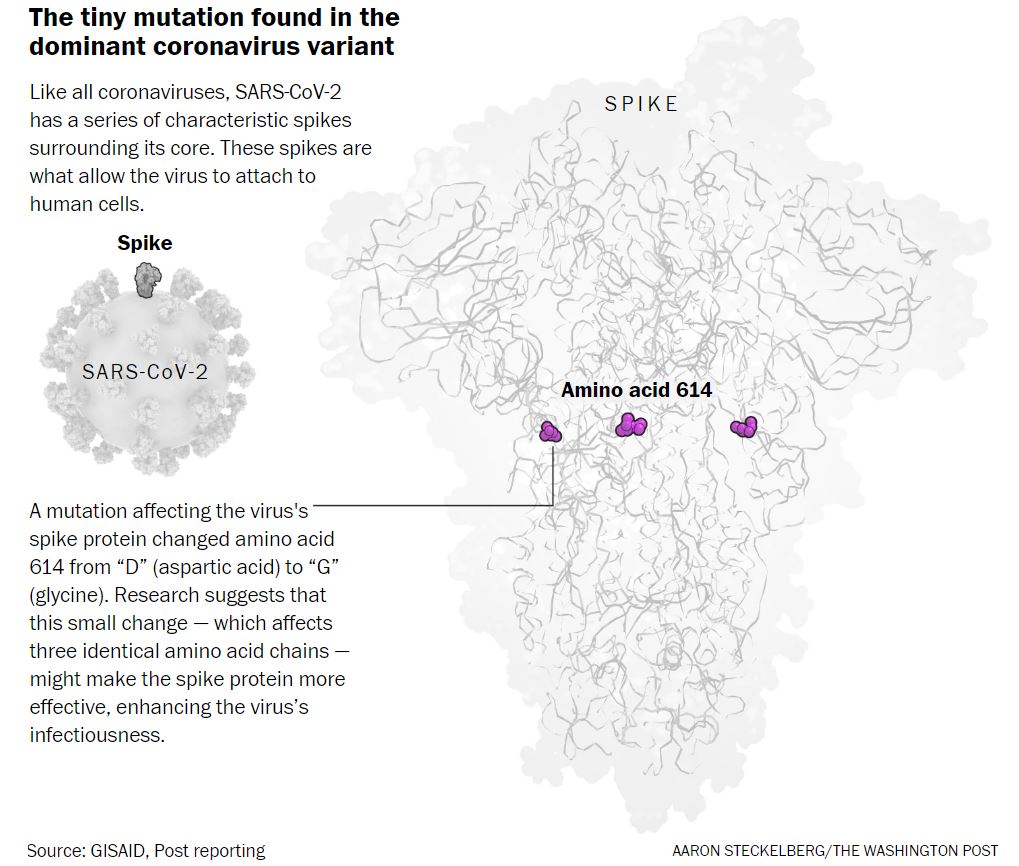
It is a SARS-CoV-2 mutation named after the position of mutation.
The amino acid shift at position 614 from D (aspartic acid) to G (glycine) produces the G614 variant of SARS-CoV-2.
It occurs on the spike protein that helps it bind to our cells, thus purportedly increasing infectivity.
More specifically, the spike protein (Surface S glycoprotein) interacts with the host’s angiotensin-converting enzyme 2 (ACE2) receptor, which is responsible for rapid human to human transmission.
The D614G-type mutation is one of the 6 major clades, and has been discovered as early as January 2020.
It is now the most prevalent form of the SARS-CoV-2 worldwide, replacing D614.
Is G614 dangerous?
Short answer: we do not conclusively know yet.
Danger in this context may be broken down to increased infectivity, increased mortality, and resistance to treatments and vaccines.
Infectivity:
In a preprint* posted on 12th June, Zhang et al. correlated greater infectivity by G614 with “less S1 shedding and greater incorporation of the S protein into the pseudovirion” i.e. hypothesising that greater stability leads to greater infectivity.
Dr. Bette Korber and his team worked on perhaps one of the greatest undertakings to track changes of the spike protein and their implications.
In their article published on 20th August, they hypothesised that the G614 variant is more infectious as it spreads more rapidly than the D614 variant, which is also consistent with laboratory findings.
They also associated G614 with higher levels of viral nucleic acid in the upper respiratory tract in human patients, which suggests higher viral loads with higher infectivity.
Mortality:
In terms of mortality, Korber et al. did not find any evidence of G614 effects on disease severity; i.e., it was not significantly associated with hospitalization status.
In a short communication article published in July, Eaaswarkhanth et al. observed that countries with the highest death tolls coincidentally have large numbers of G614 variant strains.
However, other factors should be ruled out before proving correlation or causation of G614 with increased mortality.
Will it affect future treatments and vaccines?
The spike protein i.e. the site of mutation is also a major target for treatments and vaccines. Thus, there are efficacy concerns if R&D only focuses on D614.
In a preprint* posted on 6th July, Hu et al. hypothesised that although both strains could be blocked in similar ways, there were functional differences that could affect the efficacy of therapeutics for G614:
- G614 could be cleaved by elastase-2 more efficiently, which results in better ACE2 cell infectivity
- Elastase inhibitor sivelestat sodium may partially block elastane-enhanced G614 infection
- Convalescent sera are effective for both strains, and only 7% of convalescent sera from patients with COVID-19 have reduced activity against G614
Although the D614G mutation occurs at the therapeutic target, Grubaugh et al. gathered insights from various studies and hypothesised that the mutation is “unlikely to have a major impact on the efficacy of vaccines currently in the pipeline, some of which exclusively target the receptor-binding domain (RBD)”.
There is currently no evidence to suggest the mutation will render the current proposed strategies ineffective. However, they cautioned that the mutation should still be considered in therapeutic designs.
Should I be worried about future mutations of SARS-CoV-2?
As mentioned earlier, viruses mutate as part of their life cycle. Mutations are to be expected, but we cannot reasonably predict the effects of these mutations until we identify and study them. Even then, laboratory (in vitro) findings may be different from what happens in hosts (in vivo).
There are so many factors including mutations that can drastically change the way we currently live. Instead of worrying, let’s continue to practice the new normal as per advised by MOH and WHO.
Prevention is better than cure. As the latter is absent, prevention is all the more important.
*Note: Preprints have not been peer reviewed at the time of publication.
Cover photo by Pexels