Chloroquine and Hydroxychloroquine: NOT The Magic Bullet
Exploring the possibilities of a cure for COVID-19
As Malaysians, you probably had one of these statements popping up in your conversations’ in your family’s Whatsapp chat: How to prevent disease XYZ: take herbs ABC because it has vitamin Z46 which can cure ANY disease, yadda yadda yadda.
As the world enters a third month of the reign of chaos by the coronavirus, the spread of news stating alleged “cures” for the viral infection is all over our social media, our group chats and our dinner conversations – the news, not the infection. Everything and anything has been suggested to cure coronavirus, from a telescope and a globe to warm water, and anything in-between.

However, things took a turn for the surprise when it was suggested that modern medicine may actually be the correct call this time. This Monday, President Donald Trump mentioned two drugs, chloroquine and hydroxychloroquine, stating that they have had “very encouraging early results” and saying that they are going to “make the drug available almost immediately”, which the Food and Drugs Administration also rebuffed the latter almost immediately. However, today our article will focus on two pressing questions: What are these two drugs, and can they really cure COVID-19?
What exactly are chloroquine and hydroxychloroquine?

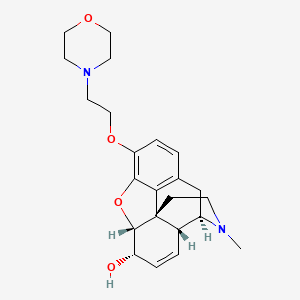
Chloroquine and its hydroxyl derivative, hydroxychloroquine, have a relatively long history. Derived from the active ingredient of the cinchona bark extract, the development of chloroquine would prove instrumental in treating malaria in the 1940s and 1950s. Today, chloroquine is indicated for malaria and extraintestinal amoebiasis (a parasitic infection of the intestines by Amoeba species), while hydroxychloroquine is indicated for malaria, lupus erythematosus and rheumatoid arthritis (auto-immune disease where the body’s white blood cells destroy other body cells, mistaking them for foreign invaders).
Chloroquine was first investigated for its antiviral properties in 2005, three years post-SARS virus (Severe Acute Respiratory Syndrome). The study showed that chloroquine inhibited SARS infection on primate cell cultures when treated both before and after being exposed to the virus, seemingly indicating that chloroquine is capable of both prevention and cure of the SARS virus.
The study deduced that chloroquine was effective for two possible reasons. The first was the effect of chloroquine on the pH of endosomes, microscope packages on the cell membranes. Chloroquine raised the pH of the endosomes, causing them to become more alkaline or basic. As the SARS virus required more acidic environments to hijack these endosomes and enter the cells, it was unable to penetrate the endosomes and subsequently infect the cells.
The second possible reason was that chloroquine affected the design of a receptor within the cells called the angiotensin-converting enzyme 2 receptor. Receptors often act as toll bridges to transport materials into and out of cells, and their unique design ensures only specific materials can pass through their toll, which includes the SARS virus. The design change brought about by chloroquine causes the toll bridge to no longer recognize and allow the SARS virus from entering the cells. Both methods have the same final result: the virus is literally locked out of the cell.
So, they can be used to treat and prevent COVID-19 infections, right?
Whoa, slow down. Even though chloroquine has been proven to treat the SARS virus, we have to bear in mind that this test was only conducted on cell cultures, and not in human subjects. The human body is a complex machine, with its unique absorption, digestion and removal system that may or may not allow chloroquine to exert its effect as well as it does on cultured cells in a laboratory.
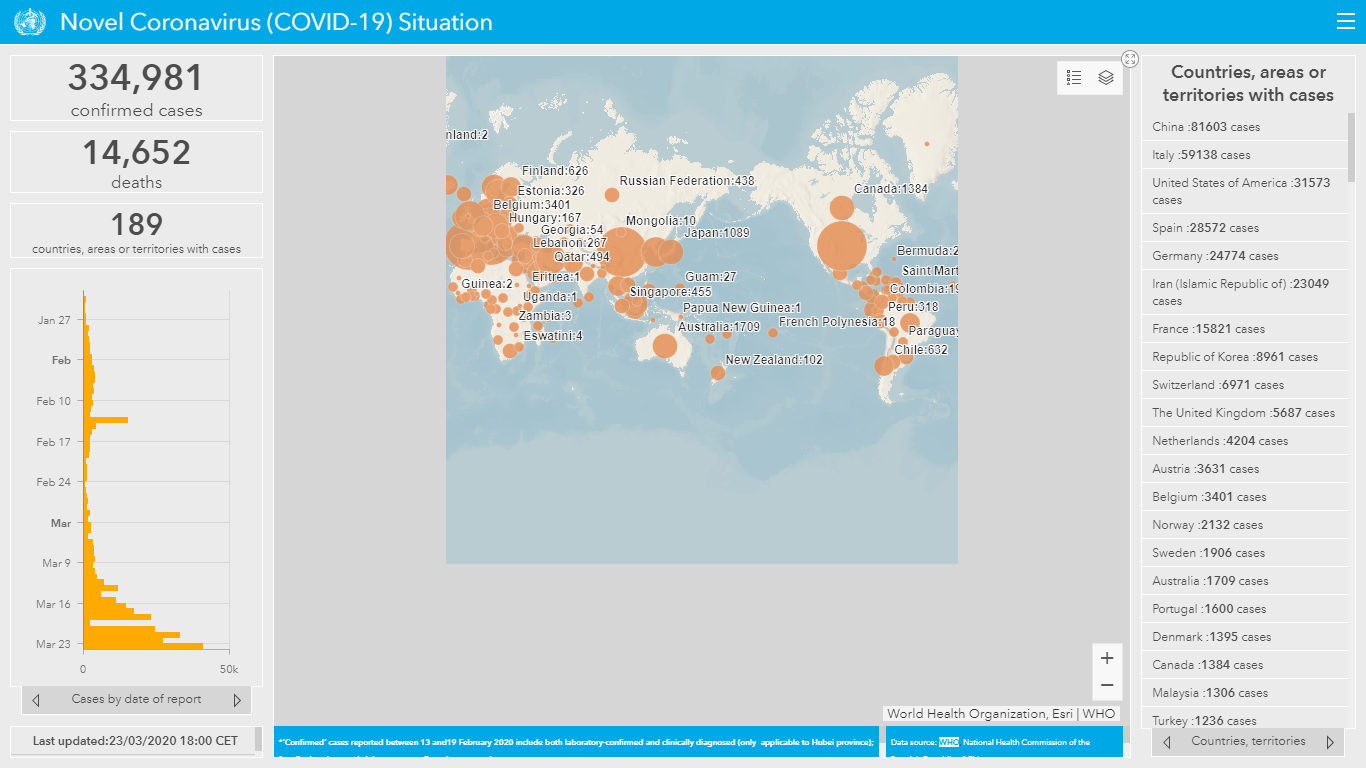
In an article by Science on March 22, WHO has included chloroquine and hydroxychloroquine as one of the four drug combinations in global megatrials to treat COVID-19 infections. In it, the WHO notes that the method that the current pandemic virus uses to penetrate and infect body cells is substantially different from SARS, and high doses of the drugs were needed to have some activity.
Why is this significant? The higher the dose, the higher the activity of the drug – but also the higher its toxicity. Within hours of President Trump’s announcement, Nigeria recorded 3 cases of chloroquine poisoning leading to hospitalization. While the reports state intense itching as one of the side effects of chloroquine, that is but the tip of the iceberg. Toxicities of chloroquine affect many body systems, including the brain (insomnia, agitation, anxiety and confusion), the liver, anaphylaxis (a severe and fatal allergic reaction) and in rare cases, fatal changes in the heart’s rhythmic beating. (Lexicomp ® Drug Information Handbook 26th Edition). This would prove true for a couple in Arizona, who found out too late after ingesting a form of chloroquine without consulting any healthcare professional.
But what about the evidence? WHO notes that while China has touted chloroquine and hydroxychloroquine as a potential life-saving drug in a test involving over 100 people, the data behind the announcement is yet to be released. Even if it was to be released, the significance of the results is still questionable as to whether it can be generalized over the entire population affected in China, let alone the world. In another study done in France, COVID-19 viral loads were decreased in nasal swabs; however, it was unclear of the effect of the treatment on clinical outcomes. In other words, the statement still lacks substantial evidence that these two drugs are key to stopping COVID-19.
Too soon to call it a “magic bullet”
Any type of medication taken without consulting a physician or pharmacist beforehand can lead to unhelpful, undesired and potentially harmful poisoning cases. There is a reason why drugs are labelled “poison” complete with skull and crossbones, a warning we need to take heed. It is too soon to conclude that chloroquine and hydroxychloroquine is the cure to the COVID-19 pandemic. Viruses mutate at an incredibly rapid pace, and there is no guarantee that even if these drugs are found effective, they will be effective for long. Thus, we do not recommend using or requesting for these two drugs as treatment as the dangers clearly outweigh the benefits. However, what we can do is to keep track of WHO’s global megatrial in order to determine a proper therapy against COVID-19, and continue to protect ourselves from COVID-19.
The opinions expressed in the article are the writer’s own and do not reflect the view of MPS YPC.