Diabetics’ Dilemma: To Puasa or Not to Puasa?
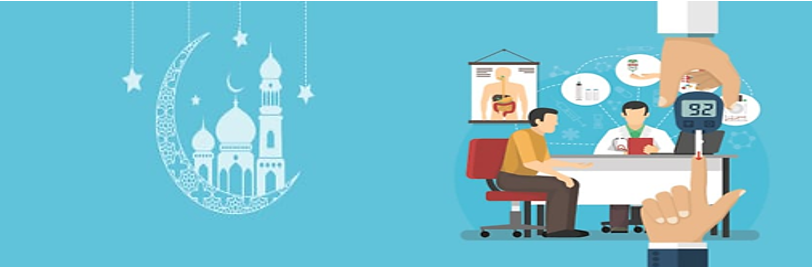
It’s the holy month of Ramadan when Muslims fast from sunup to sundown for 29-30 days. Healthy Muslims have to abstain from eating, drinking, taking oral medications, smoking and involving in sexual activities about 12-14 hours daily in Malaysia. Individuals with chronic diseases including diabetes are exempted from fasting if their condition is severe or they are deemed unfit to fast by their doctor. However, most diabetics still observe the practice of fasting. Hence, it is vital that these patients consult a health care professional beforehand to assess the risks involved and illness severity before an invidividual makes the decision to fast. It is even more important for us healthcare professionals to equip ourselves with the necessary knowledge to better educate the public.
Risks of Fasting in Diabetics
- Hypoglycaemia during fasting: A prospective study by Loke SC et al. concluded that the rate of hypoglycaemia is 1.6 times higher during Ramadan fasting amongst T2DM patients compared to non-fasting period. Diabetics are at higher risk of hypoglycaemia when taking insulin and/or insulin secretagogues.
- Hyperglycaemia: This could happen when the diabetes medication dosages are reduced excessively to prevent hypoglycaemia. Overconsumption of high-sugar food during non-fasting period can also contribute to post-prandial hyperglycaemia.
- Diabetes Ketoacidosis: Poorly controlled diabetes prior fasting month besides over-reduction of insulin dose can lead to diabetes ketoacidosis. Ketoacidosis is also more common among T1DM patients.
- Dehydration: Restricted fluid intake in addition to extended fasting period or strenuous physical activity can result in dehydration. Hypercoagulable states in diabetes can further increase risk of thrombosis and stroke.
Summary of Treatment Algorithm
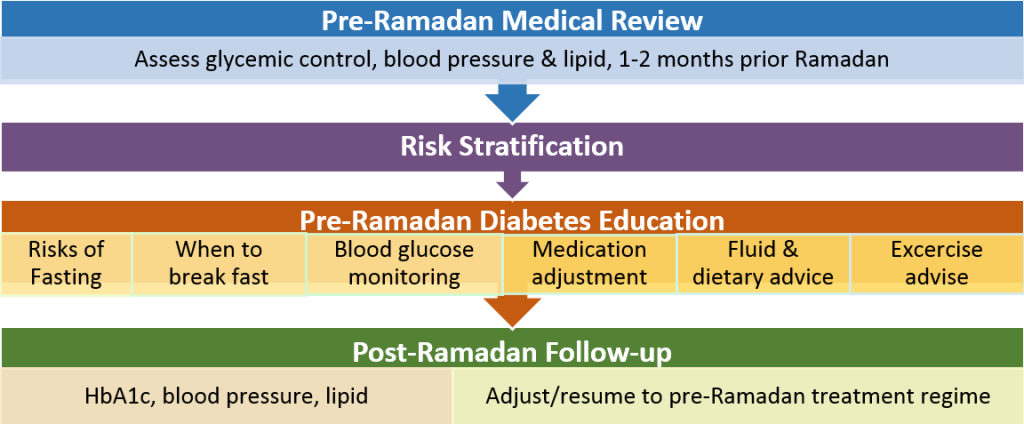
1. Pre-Ramadan Medical Review:
Diabetics should consult their doctors and/or pharmacists, ideally one to two months prior to Ramadan to assess suitability of performing fast. This is the golden opportunity for HCP to assess their detailed medical histories and current medical conditions including glycaemic control, risk of hypoglycaemia, prior Ramadan fasting experiences and self-management capabilities in order to quantify the individual’s risk.
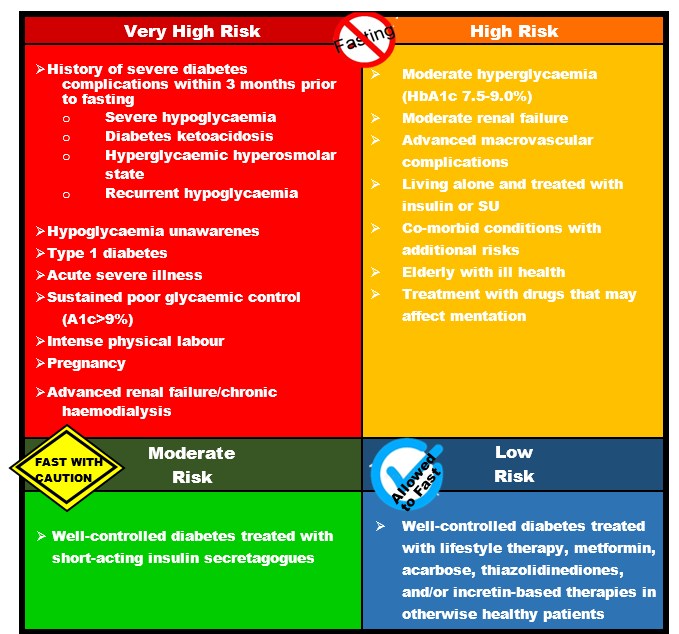
2. Risk Stratification
Assessing diabetic patient’s risks is paramount to avoid possible harmful consequences of fasting. Based on the risk categories, HCP can advise the patient to fast or not to fast. If the patient insists to fast (in particularly high or very high risk patients) individualised pre-Ramadan diabetes education should be provided to minimise the risks of complications and for optimal management of diabetes and overall wellbeing.
3. Pre-Ramadan Diabetes Education
HCPs have to proceed to this stage of providing individualised advices to patients and their caregivers if diabetic patients choose to fast regardless of their risks.
-
Risks of Fasting:
Patients should be informed that they are at higher risks of hyperglycaemia, hypoglycaemia and dehydration when fasting. Educate (or remind) them to recognise the common signs and symptoms of hypoglycaemia and hyperglycaemia.
-
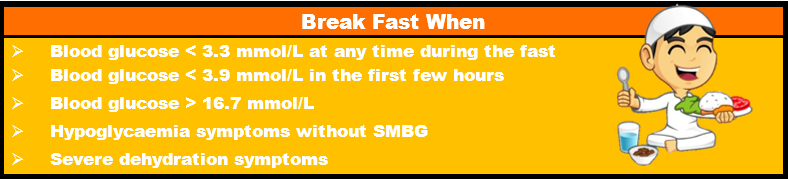
When to break fast:
When experiencing following signs and symptoms, patients should break their fast for their health’s sake. Assure them that fasting is not mandatory for the sick and alternatives like replacing the fast or paying Fidyah can be done. If hypoglycaemic, advise patients to consume simple carbohydrates. It is, however, extremely crucial that we choose to use appropriate words when we explain as we do not want to come across as insensitive or disrespectful to the patient’s religious choices.
-
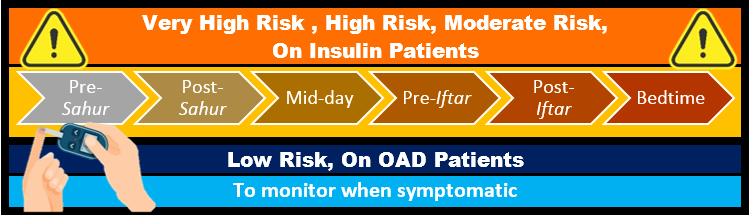
Blood glucose monitoring:
There is a misconception amongst patients that finger pricking for SMBG invalidates their fast thus skipping blood glucose monitoring. This is not the case according to JAKIM hence, correct their misconceptions, teach and remind patients to conduct SMBG as recommended to lookout for detrimental poor glycaemic control and better self-management of diabetes.
-
Medication Adjustment:
For OAD, usual morning dose should be taken during Iftar whereas evening dose is to be taken during Sahur (hey, opposite rules). Insulin secretagogues like SUs have higher risk of hypoglycaemia than insulin sensitizers hence the Sahur dose of SUs can be reduced or omitted depending on presence of hypoglycaemia episodes. For SGLT2 inhibitor, gliclazide MR and glimepride, the usual once in the morning daily dose should be converted to once in the evening daily dose during Iftar.
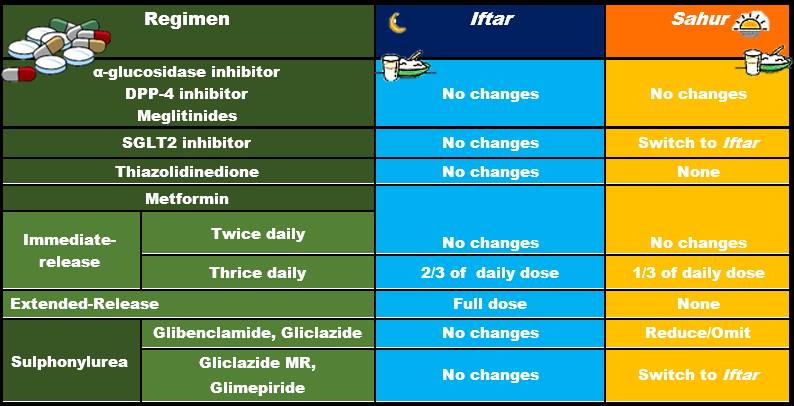
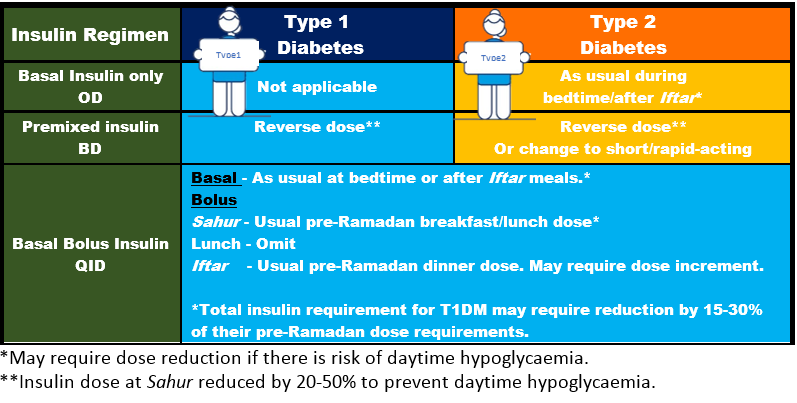
Insulin regime could be tricky but emphasizing to patient the importance of consulting treating doctor/pharmacist and regular SMBG can help to reduce the risks of hypoglycaemia and hyperglycaemia.
-
Advise on exercise, fluid & dietary intake:
Regular exercise is still important despite being low in energy. Light-to-moderate exercise and Tarawih prayers are recommended, preferably after breaking fast. Aim for 8 glasses of water during non-fasting hours to replenish fluid loss. Well-balanced nutritious food and kurma are suggested. Avoid sugary and salty food.
4. Post-Ramadan Follow-up

Definitely no one can resist the food during Raya festival especially after the month-long fasting. Remind patients that Raya is not an ‘all-you-can-eat’ ticket and eat cautiously to avoid hyperglycaemia. Follow-up consultation post-Ramadan is recommended to assess how the patient coped with fasting and also the need to readjust their medicine regimes. Due to the progressive nature of diabetes, fasting safely one year does not automatically mean that the patient is at a lower or equal risk to fast the following year, which should be emphasized to patients.
Summary: Review, Assess, Educate, Follow-up
If you’ve made it this far, give yourself a pat on the back as this was indeed a long one. Hence, to summarize, some (or most) Muslim diabetes patients may opt to fast due to religious obligations. As HCPs, we should acknowledge that and formulate individualised strategies; Review, Assess, Educate, Follow-up so that patients can fast with minimum risks.
Acronyms
CVD – cardiovascular disease
DBP – diastolic blood pressure
DPP-4 – dipeptidyl peptidase-4
HCP – healthcare professional
Hs-CRP – high sensitive C-reactive protein
OAD – oral anti-diabetics agents
PAI-1 – plasminogen activator inhibitor type-1
SBP – systolic blood pressure
SGLT2 – sodium-glucose co-transporter 2
SMBG – self-monitoring blood glucose
SU – sulphonylurea
T1DM – type 1 diabetes mellitus
T2DM – type 2 diabetes mellitus
Fidyah – food or money donations to the needy contributed by the sick/elderly/young
Iftar – sunset meal
Puasa – fasting
Sahur – pre-dawn meal
Tarawih – additional ritual prayers performed by Muslims at night after the Isha prayer
References
1) Practical Guide to Diabetes Management in Ramadan
2) CPG Management of Type 2 Diabetes Mellitus 5th Edition
3) Diabetes and Ramadan: Practical Guidelines. International Diabetes Federation (IDF), in collaboration with the Diabetes and Ramadan (DAR) International Alliance, April 2016
4) JAKIM Panduan Berpuasa bagi Pesakit, 2013
5) Recommendations for management of diabetes during Ramadan: update 2015