Monkeypox: an oncoming endemic?

We’ve just barely eased into our normal lives after the whirlwind that the last 2 years have been. So let’s just hope the title of this piece never sees the light of day for the sake of our peace of mind. However, that does not mean we should completely neglect it because although ignorance is bliss, it is never a bad idea to keep yourself well informed with the happenings of the world. And we’re here to help you do just that.
What is it?
Monkeypox is a viral zoonosis with symptoms almost similar to smallpox but is less infectious and less severe in the infected individual. This virus is a part of the orthopoxvirus genus of the Poxviridae family. It is named after the fact that it was initially discovered in a group of monkeys held in a Danish research laboratory in 1958.
Generally, it is transmitted from animals to humans through direct contact with the cutaneous or mucosal lesions, blood or bodily fluids of infected animals. Rope squirrels, tree squirrels, Gambian pouched rats, different species of monkeys are among the several animals in Africa that are known to have been infected by the monkeypox virus.
However, transmission between humans is also possible in the case of close contact with bodily fluids, lesions, respiratory droplets and contaminated beddings among others. Inevitably, that led to the first human case of monkeypox being identified in a child of the Democratic Republic of Congo (DCR) in 1970 [1]. Due to the uncertainty of its exact reservoir and virus circulation, it is recommended to avoid consumption of undercooked meat or meat of infected animals as it is a plausible risk factor.
What’s happening now
Thankfully, no deaths have been reported as of now. Nevertheless, the World Health Organization (WHO) updated on the 21st of May that among 12 of its non-endemic Member States such as Australia, Canada and Sweden, 92 laboratory confirmed and 28 suspected cases of monkeypox have been identified and are under investigation respectively.
Since the first known human case, monkeypox has been reported across central and western African countries such as Cameroon, Nigeria, Liberia and Sierra Leone. There have also been cases outside of Africa owing to international travel or animals that have been imported such as in the United States, the United Kingdom, Israel and Singapore [2]. Which is why it comes as a surprise when all the reported cases so far seem to have no travel links to an endemic area. Lucky for us, studies are well underway to understand the epidemiology, transmission patterns and the likes about the monkeypox virus.

Signs and symptoms
The incubation period (the time from being infected to the onset of symptoms) of monkeypox is usually from 6 to 13 days but can range from 5 to 21 days [3]. Monkeypox which can occur in individuals of any age is said to be self-limiting (lasts between 2-4 weeks) but the severity may be prominent in certain populations such as children, pregnant women and those who are immunosuppressed. Severity also varies based on the individual’s health status, nature of complications and extent of viral exposure.
The onset of symptoms occur in 2 defined stages:
1.Invasion period: Lasts for 0 to 5 days
-
- Fever (>38.5°C)
- Intense headache
- Lymphadenopathy (swollen lymph nodes)
- Back pain
- Myalgia (muscle aches)
- Intense asthenia (lack of energy)

2. Skin eruption phase: Occurs anytime between Day 1 to Day 3 from onset of fever
-
- Rash is more concentrated on the face and extremities
- Progresses in stages from macules to eventually papules and crusts
- Prominent areas affected:
- Face (in 95% of cases)
- Palms of the hands & soles of the feet (in 75% of cases)
- Other affected areas:
- Oral mucous membranes (in 70% of cases),
- Genitalia (30%)
- Conjunctivae & cornea (20%)

If left untreated, monkeypox can escalate to complications such as sepsis, bronchopneumonia, encephalitis, secondary infections and eventual vision loss due to corneal infection.
Treatment & Prevention
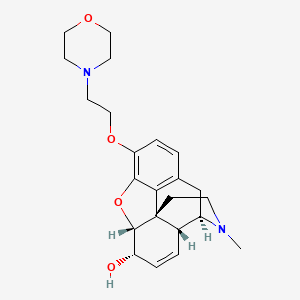
While there has been no proven definitive treatment for the monkeypox virus, the smallpox vaccine is said to be 85% protective against it and recently a monkeypox vaccine has also been developed although it has not been widely marketed yet .

Vaccinia Immune Globulin Intravenous (VIGIV) is another option in the instance where a monkeypox outbreak occurs. Primarily, it is used for treatment of complications due to vaccinia vaccination such as eczema vaccinatum and progressive vaccinia.
WHO also reported that antiviral agents, Tecovirimat and Cidofovir used in the treatment of smallpox and cowpox as well as cytomegalovirus (CMV) retinitis in patients with Acquired Immunodeficiency Syndrome (AIDS) respectively works just as effectively for controlling monkeypox outbreaks and management of its symptoms [4].
However, the vaccines are not widely available due to the fact that smallpox has been largely eradicated for some time now. Whereas the usage of the antivirals are very much on a benefit versus risk protocol with priority being given to those with severe symptoms and poor risk outcomes.
The next step
So far, there have been no cases of monkeypox reported in Malaysia and the Ministry of Health (MoH) are not planning to conduct a mass vaccination for the public as done for the COVID-19 virus. Instead, only high-risk healthcare frontliners and close contacts would be prioritised if the vaccination is to be done. They have, however, devised an adequate action plan to handle the monkeypox virus should it spread in the country. Health minister, Khairy Jamaluddin stated that a five point action plan would be set into motion when the situation calls for it [5].
The five point action plan includes:
- Early detection
- Strengthening disease diagnostic capabilities
- Case management
- Controlling outbreaks and clusters
- Increasing community awareness about the disease
Besides that, monitoring of all international flight passengers that enter Malaysia and an increase in the number and diagnostic facilities within veterinary laboratories to conduct zoonotic surveillance tests and Polymerase Chain Reaction (PCR) tests are the plans ny MoH underway in order to prevent a monkeypox outbreak.
The MySejahtera application which just recently retired from its duties during the COVID-19 pandemic is set to be reactivated from 27th May onwards to send out alerts regarding monkeypox especially to travellers coming into Malaysia from monkeypox endemic countries or countries with monkeypox cases [6]. As a preventive outbreak measure, both forward and backward tracing will be conducted together with a mandatory 21 day home quarantine to monitor for any symptoms in the affected individuals.

Additionally, the healthcare services in both government and private settings are set to cater for monkeypox screening in individuals and refer symptomatic patients to hospitals for isolation, treatment and observation.
While the government works on the bigger picture in this scenario, we can also play our part through simple preventative measures such as constantly practising good hygiene, covering our mouth and nose when coughing or sneezing, consuming only thoroughly cooked meat and avoiding any form of contact with animals or individuals that may be infected with the monkeypox virus. It’s always better to be safe than sorry. Take care and stay safe everyone.
References
- Who.int. 2022. Multi-country monkeypox outbreak in non-endemic countries. [online] Available at: <https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON385> [Accessed 29 May 2022].
- www.cdc.gov. 2022. About Monkeypox. [online] Available at: <https://www.cdc.gov/poxvirus/monkeypox/about.html> [Accessed 29 May 2022].
- Who.int. 2022. Monkeypox. [online] Available at: <https://www.who.int/news-room/fact-sheets/detail/monkeypox> [Accessed 29 May 2022].
- www.cdc.gov. 2022. Interim Clinical Guidance for the Treatment of Monkeypox. [online] Available at: <https://www.cdc.gov/poxvirus/monkeypox/treatment.html> [Accessed 29 May 2022].
- Ragu, D., 2022. No mass vaccinations against monkeypox, says KJ. [online] www.freemalaysiatoday.com. Available at: <https://www.freemalaysiatoday.com/category/nation/2022/05/26/no-mass-vaccinations-against-monkeypox-says-kj/> [Accessed 29 May 2022].
- The Star. 2022. QuickCheck: Will the MySejahtera App be used to send out monkeypox alerts?. [online] Available at: <https://www.thestar.com.my/news/true-or-not/2022/05/27/quickcheck-will-the-mysejahtera-app-be-used-to-send-out-monkeypox-alerts> [Accessed 29 May 2022].
The opinions expressed in the article are the writers’ own and do not reflect the view of MPS YPC.