HI(E)?
What is it?
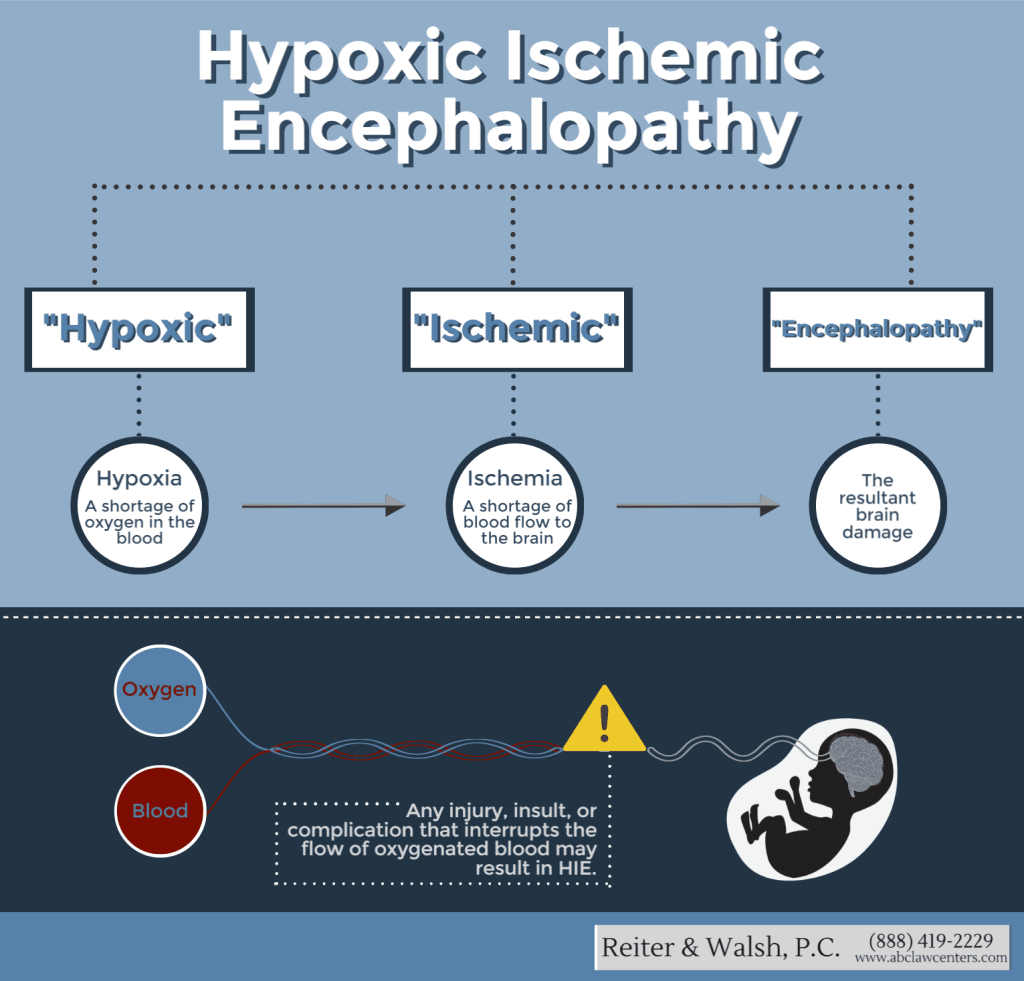
Let us break it down for you:
Hypoxic: Reduced oxygen supply to organs such as the brain
Ischemic: Lack of blood supply to the organs
Encephalopathy: Term to describe generalised brain dysfunction. As a whole, Hypoxic-Ischemic Encephalopathy (HIE) is a brain injury due to the oxygen deprivation and lack of blood flow that ensues during the prenatal, intrapartum or postnatal period. It is also known as neonatal encephalopathy, birth asphyxia and perinatal asphyxia [1].
Studies have shown that in full term infants, HIE is a serious birth complication such that 60% of infants with HIE are likely to die or succumb to severe disabilities such as epilepsy, cerebral palsy (CP) and mental retardation.
But it’s not just a condition exclusive to newborns or infants, adults are very much susceptible to HIE as well. Terms for HIE in adults include post-cardiac arrest brain injury and anoxic encephalopathy, denoting that the similarities of HIE in both populations stop at the fact that there appears to be a critical reduction of blood flow, oxygen and nutrients to the brain. Hence, making it clear that the pathophysiology of HIE is different in adults and infants.
How does it happen?
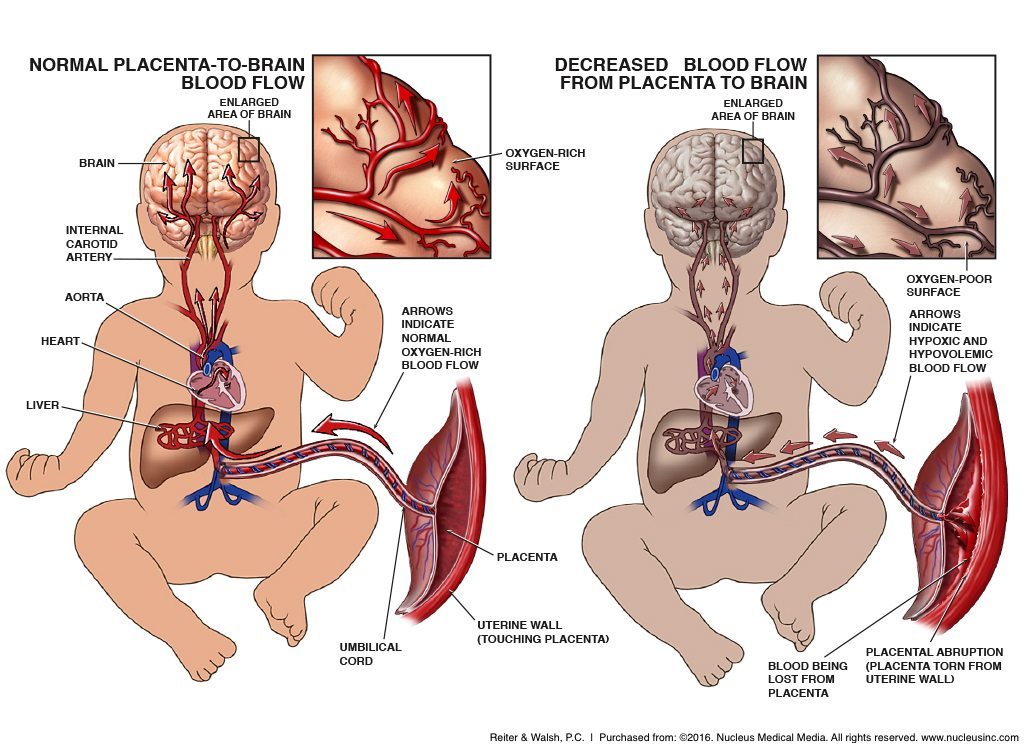
The exact cause of HIE in newborns is unknown. However, they can be attributed to the complications occurring during birth such as [2] :
- Severe foetal anaemia
- Uterine rupture
- Prolonged labour periods
- Placental abruption (Dissociation of placenta from the uterus wall)
- Excessive bleeding from placenta
- Severe prematurity etc.
In the case of adults, the lack of oxygen to the brain can be a result of health problems such as [2] :
- Cardiac arrest
- Drowning
- Carbon monoxide poisoning
- ruptured/blocked blood vessels
- Block airway due to trauma, choking, swelling etc.
- Cerebrovascular disease with secondary hypoperfusion etc.
Bear in mind that these are not the exhaustive list of HIE causes and there may be plenty more.
Signs & Symptoms
Several signs of HIE are those quite commonly seen in any newborn baby, making them difficult to distinguish as rooting from HIE itself. Among those signs & symptoms are:
- Seizures
- Breathing problems (eg. Apnoea)
- Feeding problems
- Missing reflexes
- Altered level of consciousness (eg. Hyper-alert, overly sleepy)
- Being floppy or stiff
- Irritable
- Low Apgar scores
In the case of HIE in adults, signs & symptoms include:
- Extreme tiredness
- Blue coloured skin or lips
- Breathing problems
- Loss of alertness
- Signs of seizure (eg. Muscle jerking, confusion)
Treatment options and care
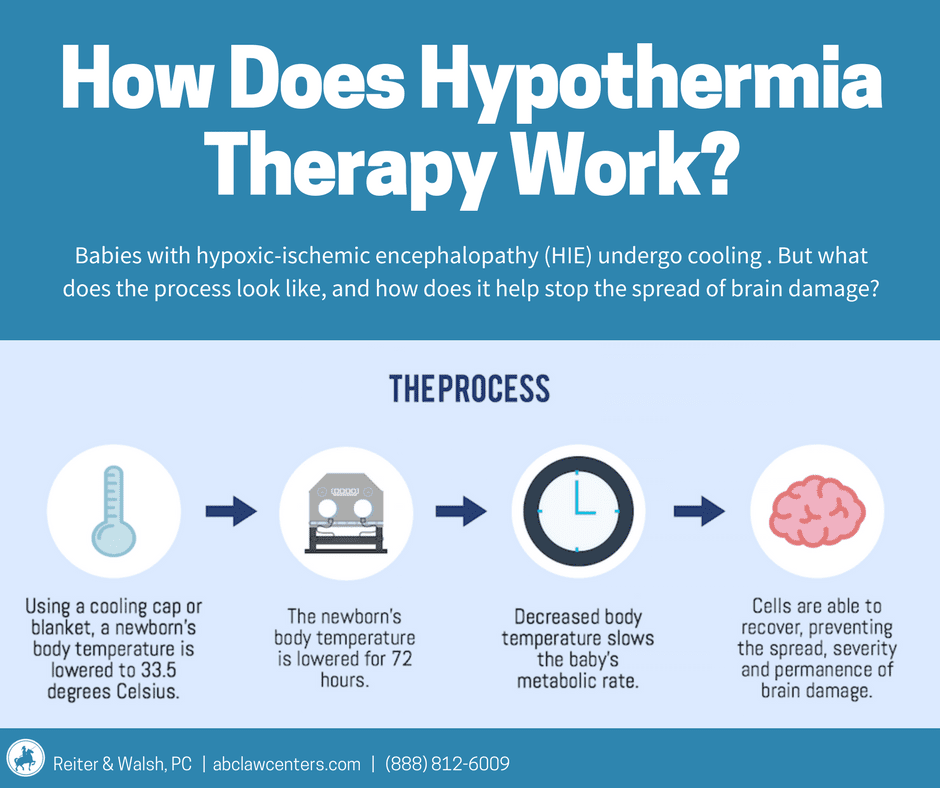
Mild HIE in babies are often quickly resolved with close monitoring to ensure they are stable. On the other hand, moderate to severe HIE is associated with death or long-lasting brain damage. Hence, therapeutic hypothermia or cooling is used to reduce such risk [2].
Usually, it is to be started within 6 hours of birth to reduce the body temperature to below normal temperature in order to retard the consequential effects of HIE. It allows for the brain to recover and reduce the extent of disability that may occur as they grow by slowing down their metabolic rate. Consequently, this helps to prevent reperfusion injury (i.e. more inflammations and release of harmful compounds) that occurs when normal blood flow and oxygenation are restored very quickly to the brain’s cells.
Supportive care is also of utmost importance. They include the likes of helping with breathing, minimising brain swelling and controlling/preventing seizures. Blood tests and monitoring of brain function through scans are also done among many other things. While these options are not curative by any means, they do help to minimise symptoms and maximise functionality.
On the flipside, treatment in adults depends on the cause of HIE and severity of brain damage. Life saving treatment such as CPR is performed if the brain stops functioning but the damage is not severe. If patients remain unresponsive even after successful resuscitation with the return of spontaneous circulations, they should be checked for initiating therapeutic hypothermia and other necessary ongoing care. Therapeutic hypothermia includes using physical surface cooling such as ice packs, endovascular temperature control devices and intravenous infusion of chilled fluids.
How does a Pharmacist fit into all this?
In the complexity of all things related to HIE, medication reconciliation may not strike as something crucial. However, it can make a lot of difference if you think about it. The work entails a pharmacist mainly to obtain and document the complete list of medications that the patient is currently on and comparing it to that which the patient was previously on (either during transfers from hospitals or upon discharge). The idea behind it is that the pharmacist will be able to verify that the patient is on the appropriate medications for their current condition and identify if any changes or interventions need to be done to accommodate said current condition.
Medication reconciliation at its core involves communication and cooperation among the healthcare team involved in caring for a patient. For example, if a patient is transferred from a district hospital to a central hospital, chances are that the patient/ patient’s family did not bring along the patient’s medication or current prescription with them.
In such cases, it is often the pharmacist’s duty to liaise with the healthcare team from the district hospital to reconcile the patient’s medication so that he/she does not miss out on their usual medication regimen. Thus, allowing for the patient’s comorbidities to be treated accordingly and not further worsen their condition. Additionally, if the patient’s current condition calls for a more intensive or subdued therapy, the pharmacist can identify the appropriate treatment upon discussion with the medical team. Surely, this would also be an opportunity to identify and resolve any discrepancies in the patient’s treatment [3].
Furthermore, while there are not many references on what kind of supportive care pharmacists can provide for an ailing HIE patient, it is a given that pharmacists would provide counselling to the patient, caretaker or their family member on any medication or device that is necessary. For patients on mobility devices, referral to a physiotherapist might be the best option as optimising their movement with the aid is the main goal. On the other hand, for newborns and babies, the care and management involved is very intricate as they are delicate. As such it is crucial that the supportive care given to them by the healthcare team is done attentively to avoid any errors or potential mishaps. One such guideline available is the HIE Supportive Care Management Guidelines.
Then what?
Some babies are lucky to recover from HIE unscathed but some would face long term issues that require the help of speech therapists or physiotherapists. A lot of care and attention must be put into the baby’s behaviour and progress especially those related to their motor, cognition, sensory and language developments. Obviously plenty of assessments must be done over time to gauge the child’s development and to address any concerns that may arise. However, it is advisable for the parents and family of the child to discuss and communicate with the healthcare team so as to understand the prospects that lie ahead without overwhelming themselves.
As for adults, supportive and preventive care is a major part of the HIE therapy. Along with that, efforts must be made to ensure they receive sufficient nutritional support, reduce chances of nosocomial infection and ensure adequate prophylaxis for venous thromboembolism. It is important that family members of patients with severe neurologic injuries are informed about the patient’s prognosis in order for the best course of treatment to be decided while taking into consideration the patient’s wishes.
We hope you all know a little more about HIE now. It’s not pleasant to be having any kind of condition, be it physical or mental. So, be kind whenever you can 🙂
Reference
- Bliss. (n.d.). Hypoxic-ischaemic encephalopathy (HIE). [online] Available at: https://www.bliss.org.uk/parents/about-your-baby/medical-conditions/hypoxic-ischaemic-encephalopathy-hie.
- www.abclawcenters.com. (n.d.). Hypoxic-Ischemic Encephalopathy (HIE): Legal Help for Birth Injuries. [online] Available at: https://www.abclawcenters.com/practice-areas/prenatal-birth-injuries/fetus-or-newborn-medical-problems/hypoxic-ischemic-encephalopathy/.
- Duguid, M. (2012). The importance of medication reconciliation for patients and practitioners. Australian Prescriber, [online] 35(1), pp.15–19. doi:10.18773/austprescr.2012.007.







