Medicines Originated From Plants – Quinine and Artemether for Malaria

Prologue – Malaria
Malaria is the product of the plasmodium parasite, carried by several species of Anopheles mosquitoes, which spreads when they sting their hosts.2 Once entered the human body via saliva from mosquito bites, the plasmodium parasites will invade the liver. P. falciparum, predominantly found in Africa, is the most lethal of all strains. P. vivax is prevalent in all other countries besides countries in the African continent. The other plasmodium species that target humans include P. ovale and P. malariae.2 P. knowlesi, which used to be a simian infection, is the latest addition to the family.2 P. vivax and P. ovale are a handful to handle in particular, as they can form hypnozoites, which remain latent in the host for months and sometimes even years.6 Prevention of malaria can be classified into suppressive prophylaxis and causal prophylaxis.2 In severe cases of malaria, infusion of artesunate is preferred.2
A Miracle Cure in the New World – Quinine
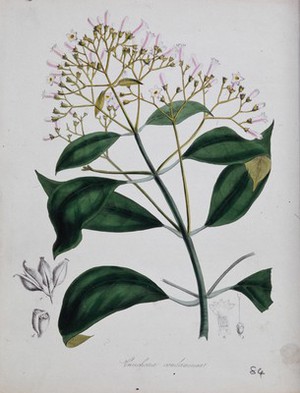
Also known as ‘The Jesuit Bark,’ quinine’s discovery has blessed the people plagued by malaria.4 Quinine is extracted from the bark of cinchona trees found in the southern American region. It is particularly effective against the two plasmodium species that cause malaria, P. falciparum and P. vivax.4 In cases of overdose, the adverse effects were collectively described as “cinchonism”.4 The symptoms include tinnitus, nausea, headaches, dizziness, and disturbed vision.4 In rare and severe cases, high doses of quinine will backfire and result in another condition called blackwater fever or malarial hemoglobinuria.4 Blackwater fever obtained its name from its ability to cause the victims to pass out dark red blood due to quinine’s mass destruction of red blood cells.1 The victims will develop anemia quickly, leading to rapid pulse and fatigue due to low blood volume.1
Not long after the widespread use of quinine, resistance starts to rear its ugly head.1 Luckily and at the same time, unluckily for the colonized, research funding poured in to fund the scientists trying to synthesize quinine derivatives with better properties as a cure for malaria is the key to continue conquering the equatorial region.1 When the parasites have gotten the better of the synthetic derivatives, chloroquine and primaquine, the world is waiting for another breakthrough that can save the lives of people plagued by mosquito-borne malaria, which happened in 2015.
Looking Beyond the Quinine Derivatives – Artemether
Artemether belongs to the Artemisia family, a popular antimalarial in ancient China.4 Known as ‘Qinghao’ (青蒿) in Chinese, the extract from sweet wormwood was included in the “A Handbook of Prescriptions for Emergencies” (肘后备急方) by Ge Hong (葛洪), which was compiled in the Jin Dynasty. The scientist Tu Youyou, who unearthed the potential of the herb from ancient Chinese text, earned herself the Nobel Prize in Physiology or Medicine in 2015. Today, artemether combined with lumefantrine (also known as benflumetol) under the brand name Riamet is the first-line treatment for uncomplicated P. falciparum infections.2 Together, they interfere with the conversion of haem to non-toxic haemozoin in the food vacuoles of the parasites.2 They also inhibit the parasites’ DNA and protein synthesis.2 The other combination includes:
• artesunate-amodiaquine (AS+AQ)
• artesunate-mefloquine (ASMQ)
• dihydroartemisinin-piperaquine (DHAP)
• artesunate + sulfadoxine-pyrimethamine (AS+SP)
• artesunate-pyronaridine (ASPY)
The resurfacing of the old medicine has solved the problem of widespread resistance of plasmodium towards quinidine and its derivatives.7 However, resistance to artemether is also emerging, especially in the P. falciparum strain.2,7 Artemether monotherapy and sub-standard antimalarials are strongly discouraged as a countermeasure for the brewing resistance towards artemether.2,7 Instead, an artemisinin-based combination therapy (ACT) should be used as a standard treatment for uncomplicated P. falciparum infection and suspected chloroquine-resistant cases.2,7

Epilogue – The beginning and the endless fight
The purpose of this article is to remind us to appreciate the development of modern medicine, allowing us as pharmacists to have many tools in our list of drugs. As we can see, the development of each medicine has come a long way. Hence, we should be grateful for the efforts of our predecessors by learning how to dispense medicine wisely. The knowledge is already laid in books. After all, all we need to do is to take it from the hard work of those before us.
Fun fact:
The poison diethyltoluamide (DEET) 20-50% can be applied safely if the babies are more than two months old as a mosquito repellant. Due to possible poisoning, DEET may be used under two months old but with caution. The large surface area to body mass ratio increases the rate of absorption of DEET, resulting in toxic levels. 2
- Britannica, T. Editors of Encyclopaedia. Blackwater fever [Internet]. Chicago: Encyclopedia Britannica; 2022 Aug 12 [cited 2023 Jan 15]. Available from: https://www.britannica.com/science/blackwater-fever
- Clinical Practice Guideline: Management Guidelines for Malaria in Malaysia, 3rd Edition. Putrajaya: Ministry of Health, Malaysia; 2014.
- Liao F. Discovery of Artemisinin (Qinghaosu). Molecules [Internet]. 2009 Dec 21;14(12):5362–6. Available from: http://dx.doi.org/10.3390/molecules14125362
- Peter Macinnis. A Brief History of Poisons: From Hemlock to Botox and the Killer Bean Calabar. New York: Arcade Publishing; 2011.
- Press release. NobelPrize.org. Nobel Prize Outreach AB 2023. Sat. 7 Jan 2023. Available from: https://www.nobelprize.org/prizes/medicine/2015/press-release/
- Tu You You. Artemisinin—A Gift from Traditional Chinese Medicine to the World. 2015 Dec 7. Available from: https://www.nobelprize.org/uploads/2018/06/tu-lecture.pdf
- World Health Organisation. WHO Guidelines for Malaria [Internet]. Geneva: World Health Organization. 2022 Nov 25 [cited 2023 Jan 15]. Available from: https://files.magicapp.org/guideline/dfdf0878-bfdd-444b-a319-5ae9f50b1154/published_guideline_6832-5_6.pdf







