Behind The Counters Of Out-patient Pharmacy

Did you know, government dispensaries always ensure their patient waiting times never exceed a total of 30 minutes?
In 2008, the Ministry of Health implemented a key performance indicator (KPI) target of only 30 minutes of waiting time in government dispensaries and pharmacies. Within a year of introduction, 93% of hospitals and health clinics achieved this target. In other words, approximately 95.4% out of a total of 39.4 million outpatient prescriptions were dispensed within the targeted time [1].
While some may say half an hour is a reasonable wait time, some still argue that it’s ridiculous. Before taking your stand, let’s zoom in closer to the outpatient pharmacy and all associated activities.
What Is Out-patient Pharmacy?
Outpatient is a division of the hospital pharmacy department involved in four main processes: screening, filling, counter checking and dispensing. Each stage in the outpatient setting is uniquely important in preventing medication error and consequently protecting patient safety.
Screening
The first part of out-patient pharmacy begins when you hand over your prescription to the screening pharmacist. The pharmacist would screen the prescription to verify its validity and safety.
Pertinent information such as patient name, RN number, medication regimen and indication, and prescriber signature will be checked [2]. The screening pharmacist would also look for drug-drug interactions, contraindications or incompatibilities.
The pharmacist-in-charge would clarify any ambiguity or error in prescriptions with the prescriber before being passed over to the next stage. Once the prescription is deemed safe for dispensing, the screening pharmacist will pass it to the next step—labelling and filling.
Labelling & Filling
Labelling of drugs is essential to ensure that the medicine is clearly and easily identifiable by health professionals and consumers [3]. This helps avoid confusion or mix-ups during dispensing and at home when patients are on their own.
At this stage, pharmacists should fill medications for patients according to their labels and prescription. Every patient is different, and so are their prescription and requirements. Therefore, pharmacists must meticulously assess each prescription to ensure the right drug, dose, and amount are being filled.

Some prescriptions even require extemporaneous preparation of medicines for products that are not commercially available. Pharmacists must check the suitability and stability of the product for extemporaneous preparation. Followingly, the extemporaneous preparation of medicine must be performed according to evidence-based references and in line with the standard Good Preparation Practice.
Furthermore, prescriptions requesting dangerous drugs such as oxycodone (a common opioid painkiller) or benzodiazepines (a psychotropic drug) require a few additional steps before dispensing. This is because the process of dispensing dangerous drugs must be in accordance with the Dangerous Drug Act 1952.
Pharmacists must check the prescription to ensure authorized personnel prescribes the dangerous drug. Then, the pharmacist involved in dispensing the dangerous drug should document information about the dangerous drug in writing.
Once a prescription is filled, the pharmacist must sign it with their initials to declare accountability for any errors or clarifications.
Counterchecking
As the name suggests, this stage of outpatient pharmacy involves checking the filled medications for any near-miss errors. Near-miss errors describe an act of negligence that could have harmed a patient but, fortunately, did not cause harm due to prevention [4]. In cases where errors are detected, the pharmacist that signed off the prescription would be called to amend their mistake.
Dispensing
This is the final stage in outpatient pharmacy, and it’s one of the most important because it’s the last point of contact with the patient. The dispensing pharmacist is responsible for checking the 5 Rights on Quality Use of Medicines (QUM):
- Right patient
- Right medication
- Right dose
- Right time
- Right route of administration
When dispensing the medication on the counter, the pharmacist must ensure adequate counseling is provided to the patient. The teach-back method would be implemented in some cases to ensure the patient understands how to take the medication. The pharmacist would attempt to clarify any patient questions too.
The Importance Of Out-Patient Pharmacy
Medication errors are one of the most concerning threats in our healthcare system. But the good news is, they’re totally preventable!
Pharmacist interventions are necessary to identify and resolve prescription errors to achieve optimal therapeutic outcomes for the patient. You can visualize the importance of the outpatient pharmacy department using The Swiss Cheese Model of Accident Causation.
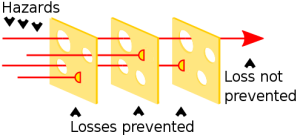
Imagine each layer of cheese as the different processes within the outpatient department. Pharmacists’ intervention in each step ensures that medical errors are spotted, resolved and prevented from reaching the patients.
The outpatient pharmacy also allows interdisciplinary communication between pharmacists and healthcare providers. Collaborative decision-making is integral in bringing out the safest treatment plan for patients.
Factors such as the number of prescriptions, availability of staff and pharmacist and intervention requirements could potentially contribute to a longer waiting time.
Conclusion
Many perceive pharmacists solely as people who receive prescriptions and dispense medications. But pharmacists are all that and so much more. Outpatient pharmacists ensure you get to bring back the safest medications home.
While waiting in the hospital chairs for a prolonged period is definitely frustrating, the hassle of experiencing a medication error is far worse. So, next time, before grunting impatiently at the outpatient department, we kindly hope this article helps you understand that there’s much more going on behind the counters.
References:
- Fahrurazi, F. E., Ibrahim, N. H., Mafauzy, N. M., et.al (2022). Factors affecting waiting time in Outpatient Pharmacy at Hospital Raja Perempuan Zainab II (HRPZ II). Journal of Pharmacy, 2(1), 1-7. doi: 10.31436/jop.v2i1.105
- Record of Training and Experience for Provisionally Registered Pharmacist. (n.d.). Retrieved from https://www.pharmacy.gov.my/v2/sites/default/files/document-upload/out-patient-pharmacy-services-2019.pdf
- Siew Siang, C., Ni, K., Noor, M., & Ramli. (2003). Outpatient Prescription Intervention Activities by Pharmacists in a Teaching Hospital *Author for correspondence. Malaysian Journal of Pharmacy, 1(3), 86–90. Retrieved from https://www.mps.org.my/publications/Journal_of_Pharmacy3/research_paper2.pdf







